Stewardship, Stewardship, Stewardship
There has been a plethora of antimicrobial stewardship scholarship published these past few weeks. I'm currently on the inpatient medicine service and have even been harassed by the antimicrobial stewardship team (humor), so I only have a moment to briefly highlight three can't miss articles:
(1) Manisha Juthani-Mehta and co-authors just published an excellent JAMA Viewpoint discussing Antimicrobials at the End of Life. It is open-access (free), so I hope you have a chance to read it thoroughly, but the main points include:
(2) Dan Livorsi and colleagues at the Sidney and Lois Eskenazi Hospital and the Richard Roudebush Veterans Affairs Medical Center in Indianapolis just published an important qualitative study in September's ICHE of factors that influence antibiotic prescribing among inpatient physicians (10 resident and 20 staff physicians). I'm happy to add that Dan Livorsi has just joined our group in Iowa City, where he is helping to jump-start our stewardship programs. Key findings of his study include:
(1) Manisha Juthani-Mehta and co-authors just published an excellent JAMA Viewpoint discussing Antimicrobials at the End of Life. It is open-access (free), so I hope you have a chance to read it thoroughly, but the main points include:
- "Evidence-based and goal-directed counseling about infection management at the end of life must be a routine part of advance care planning and treatment discussions between clinicians and patients with advanced illness."
- "Clinical algorithms aimed at improving antimicrobial stewardship from an infectious disease standpoint must also integrate treatment preferences when applied to patients near the end of life."
- "To the extent that inadequate outcome data hinder decision making, researchers should consider whether there is adequate clinical equipoise and need to justify a carefully designed randomized trial comparing symptom control and survival among patients with advanced illness who receive antimicrobials vs high-quality palliative care for suspected infections."
(2) Dan Livorsi and colleagues at the Sidney and Lois Eskenazi Hospital and the Richard Roudebush Veterans Affairs Medical Center in Indianapolis just published an important qualitative study in September's ICHE of factors that influence antibiotic prescribing among inpatient physicians (10 resident and 20 staff physicians). I'm happy to add that Dan Livorsi has just joined our group in Iowa City, where he is helping to jump-start our stewardship programs. Key findings of his study include:
- "Antibiotic overuse is recognized but generally accepted;
- the potential adverse effects of antibiotics have a limited influence on physician decision making;
- physicians-in-training are strongly influenced by the antibiotic prescribing behavior of their supervising staff physicians; and
- other physicians’ prescribing decisions are sometimes questioned, but there is limited peer-to-peer feedback or critique."
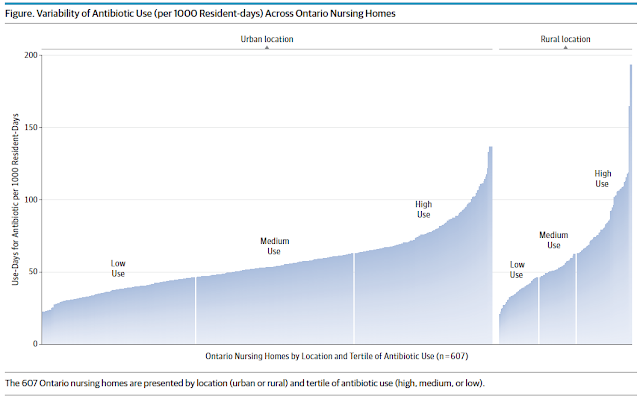
(3) Nick Daneman and colleagues in Ontario examined antibiotic use and secondary harms in 607 nursing homes housing 110,656 residents in a recent JAMA Internal Medicine. Their findings are quite striking (if not surprising) in that antibiotic use varied from a low of 20.4 antibiotic days to a high of 192.9 antibiotic days per 1000 resident days. Antibiotic-related adverse events were higher in "high-use" nursing homes even among patients who did not receive antibiotics. An interesting finding (for someone in Iowa) was that rural facilities were overrepresented in the highest tertile of antibiotic use (see figure below), but after accounting for other nursing home– and patient-level characteristics, rurality was found to be protective against antibiotic-related harms." Would be interesting to figure out why rurality is associated with higher antibiotic use but fewer harms but my guess is that rural folks are just awesome. Of note, Lona Mody and Chris Crnich published an accompanying editorial that is worth reading.

Comments
Post a Comment
Thanks for submitting your comment to the Controversies blog. To reduce spam, all comments will be reviewed by the blog moderator prior to publishing. However, all legitimate comments will be published, whether they agree with or oppose the content of the post.